Kris Van de Poel, University of Antwerp, Belgium and North West University, South Africa
Christine Fourie, Stellenbosch University and North West University, South Africa and University of Antwerp, Belgium
Karen Seberechts, University of Antwerp, Belgium
Van de Poel, K., Fourie, C. & Seberechts, K. (2013). Medics on the Move South Africa: Access to medical words. Studies in Self-Access Learning Journal, 4(4), 339-352.
Download paginated PDF version
Abstract
South African medical students who are Cuban-trained and therefore Spanish- speaking, on their return to South Africa need to learn medical vocabulary, terminology, and appropriate interactional discourse in the two major languages of English and Afrikaans, in order to be able to practise professional medicine effectively and efficiently. Indeed, their language problems are further compounded by differences in medical equipment and in medical practices between Cuba and South Africa. To meet these particular students’ needs and provide a communication support tool, the concept of a paper-based pocket-size multi-lingual illustrated dictionary was introduced as an additional component in a blended learning approach, to complement online materials called MoM-SA. The dictionary, to which students are invited to add material, has word lists in English, Afrikaans and Spanish, and offers links to the online materials. Students can add terminology, translations into other African languages and images, so that the dictionary grows and reflects the everyday needs of the students, who, at the same time, become co-owners of the dictionary; thus, process has become content and, as a result, learner motivation has increased.
Keywords: medical terminology, medical discourse, communication support tool, multilingual medical practice, ESP, MoM-SA
Setting the Scene: Cuban-Trained South African Medical Students
With eleven official languages, communication challenges in a multilingual South African (SA) professional healthcare context are manifold. Medical professionals are expected to communicate in different languages depending on the region where they operate. In the Western Cape province, for instance, they are expected to communicate in English, Afrikaans and isiXhosa, the three dominant languages in the region. Since medical students apply to a school which may not be in the area where they were raised, they are very often challenged with having to learn another language in which to function professionally. Moreover, it is by no means certain that they will have been schooled in both Afrikaans and English, as well as another African language. First year medical students at the University of Stellenbosch therefore sit language proficiency tests when they enter university and have to take part in an academic literacy course in either English or Afrikaans, whichever has proved to be their least strong language. Apart from this academic literacy course, the students also have to complete a communication course in their weakest language, between the two languages of isiXhosa and Afrikaans.
However, an altogether different linguistic challenge came about in 1985, when South Africa and Cuba signed a cooperative health agreement as part of an intervention which seeks to address the shortage of qualified medical doctors in South Africa (Health Care in South Africa, 2013).
Through the programme, on an annual basis, a group of medical students from South Africa, who have not passed the entry requirements to medical school, are allowed to spend the first six years of their training in Cuba. During this period the students receive twelve months of intensive Spanish language training, followed by five years of medical training (undertaken in Spanish in a prevention-oriented health care system). Upon their return to South Africa, the students are admitted to different universities where they do their internships and complete their studies, undertaking the Cuban final qualifying exam which is ratified in South Africa.
At Stellenbosch University, where the participants in this study were enrolled, the intensive orientation programme, which has been designed for them as a group, with their specific needs in mind, consists of 1) medical skills training appropriate to curative-oriented health care, 2) language courses with a focus on medical communication in English and Afrikaans (the two major languages for professional medical communication in the Western Cape region of South Africa) and 3) supervised clinical ward rotations in the university hospital.
Since these medical students, whose home language is often not English or Afrikaans, but who may have been schooled in one of these languages, have undertaken all of their medical training in Spanish, they have learned the medical vocabulary as well as more general medical communication practices only in Spanish. Consequently, in order to be able to communicate and practise medicine effectively in South Africa, they need to (re-)learn the medical vocabulary and terminology, as well as related interactional discourse or scripts.
Medics on the Move and Medics on the Move South Africa (MoM-SA)
Since quality of doctor–patient and doctor–colleague communication can directly influence the quality of patient care (Hewett, Watson, Gallois, Ward, & Leggett, 2009; Watson, Hewett, & Gallois, 2012) and may even improve patient health outcomes (Stewart, 1995), communication training has, in recent years, received ample attention in patient-centred medicine. Even though it has become an integrated component of a western medical curriculum, language support guides (such as the Calgary-Cambridge guides; Silverman, Kurtz, & Draper, 2005) ‘typically mention the use of a second or foreign language as just one of many issues in cross-cultural communication without providing any solutions or prescriptions to address ensuing communication problems’ (Gasiorek & Van de Poel, 2012, p. 4).
This need to address the issue of cross-cultural communication for medical professionals has led to the development of Medics on the Move (MoM). Medics on the Move started in 2006 as an EU co-funded project and has since developed into an online tool for six European languages at beginners (MoM-basic) and advanced level (MoM-advanced) with translation support for six other languages (www.medicsmove.eu). MoM is intended for (pre-)professionals to use autonomously as a communication tool in clinical settings, but it can also be used as a learning tool in training and teaching contexts.
The online materials for beginners (MoM basic) are based on scenario texts which follow the doctor-patient consultation timeline interspersed with communicative situations with colleagues. The syllabus is functional and speech-act-based and the scenario texts have different types of support: phonetic (audio and systematic pronunciation training), grammatical (rule-based with examples from medical contexts), lexical (wordlist and wordmaps bringing words together in semantic fields) and communication (a task-based approach, see below for more examples).
Due to the communication challenges for the students in a South African medical professional setting and the fact that SA medical schools have integrated patient-centred communication in their medical training programmes, the Faculty of Medicine and Health Sciences at Stellenbosch University introduced a language-specific communication training programme for all students. Given the complex profile of the learners, the restricted number of teaching hours and the lack of targeted teaching and learning materials, the approach adopted in the developmental process was critical. The programme was conceived, in 2013, as a collaboration between the Language Centre and the Medics on the Move team, with input from local developers, pedagogues, material designers and medical consultants. It has adopted a blended learning approach (Graham, 2006) consisting of (limited) contact teaching (20h) and autonomous online learning (see, among others, Little 1991) and is tailored for a South African context for online and contact teaching and learning both in Afrikaans and English[1]. In order to inform the programme, called MoM-SA, a needs analysis was carried out involving staff and students. Since the Cuban-trained students have special needs, they were studied separately.
Needs Analysis as Part of MoM-SA Implementation
In 2012, after having completed the medical training programme in Cuba and having participated in the medical orientation programme, a group of ten Cuban-trained SA students[2] took part in a needs analysis (questionnaire and focus group) that was conducted with a view to increasing learning output (Van de Poel & Gasiorek, in press). Students reported reversed culture shock with respect to South African culture and clinical contexts (Szkudlarek, 2010), in terms of personal and medical experiences, as well as language skills. Students explained, among others, that they had to get used to the food cooked at home and they often felt estranged from their families and friends, but, specifically, they had difficulties with professional communication, and, more particularly, with understanding and using medical terminology in English and Afrikaans. The overall findings, with respect to medical communication, were that these pre-professionals suffer from the threat of losing face when trying to be the doctors they want to be.
One of the major linguistic preconditions was that students had to make their own notes and vocabulary lists in order to cope with their own deficient medical language skills while on ward rotation. Moreover, the difficulties with terminology were compounded by differences in medical equipment and medical practices between Cuba (focused on primary healthcare, i.e. prevention) and South Africa (focused on secondary or curative care). Students were at a loss and claimed, “You find yourself in a ward and almost everything that you see you don’t know what it is because the equipment is different” or “you don’t know what it is called”. The same holds true for the use of abbreviations which students experienced as “secret codes” that make life “complicated”. Needs analysts concluded that the students’ lack of vocabulary and specific terminology should be systematically addressed. Students themselves hint at a possible solution, “We know the Spanish medical terms, but it is English now” (responses as reported in Van de Poel & Gasiorek, in press).
On the basis of the findings it was decided to introduce the Cuban-trained students to MoM-SA materials and engage them in blended learning; however, clinical settings are not always predictable and can therefore not be learned entirely as pre-patterned chunks. To meet the students’ particular linguistic and communicative needs and to get them involved in creating their own learning content, the MoM-SA team sought to develop the optimal cocktail of blended learning communication support.
MoM-SA’s Missing Link: a Pocket Size Dictionary
The online version of MoM-SA and the course book derived from it contain ample opportunities to learn, internalise and extend general and specialised medical vocabulary at a basic level. Lexical items are presented in the context of a written scenario, with audio support and translation into six languages (for the basic course the topics covered are Greeting, Examining and instructing, History taking, Symptom analysis, Case presentations, Emotions, Explaining results, The management plan, Planning and Problem solving. See Figure 1 for the different components of one unit taken from the English MoM).
Figure 1. Overview of Unit 1 Content
Words are presented as part of scenarios and can be looked up in an online wordlist which contains audio, grammatical information, carrier phrases and translations (see Figure 2 for an extract of a scenario text of the first unit in English and Figure 3 for a lemma from the online wordlist in English).
Figure 2. Scenario Text of Unit 1: Where Do You Come From?
 Figure 3. One Entry from the MoM-basic Wordlist
Figure 3. One Entry from the MoM-basic Wordlist
To effectively foster contextualised learning, the words and terms are also arranged in interactive wordmaps where they are grouped by topic/semantic fields, as shown in Figure 4 (Swanepoel & Van de Poel, 2002).
 Figure 4. An Interactive Mindmap on the Health Care Team (the red links refer to the wordlist)
Figure 4. An Interactive Mindmap on the Health Care Team (the red links refer to the wordlist)
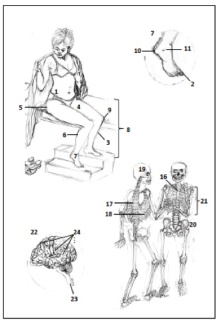
However, as pointed out above, the need for extra on-the-job support was accentuated when students went on ward routines and struggled to communicate with patients and medical staff. Consequently, the concept of a pocket size dictionary was developed containing general medical words as well as medical terms and supported by images and drawings (Van de Poel & Seberechts, 2013). Following the requirements set out in Swanepoel and Van de Poel (2002), the communication support tool was arranged as illustrated multilingual word lists containing English, Afrikaans and Spanish, reflecting the contexts that students encounter. To effectively foster contextualised learning, the words and terms were grouped per topic.
Learning was guided by presenting words in subfields, systematically presenting the words as linked to the drawings. For reasons of saliency, the words were ordered alphabetically in Spanish. Moreover, a fourth column was introduced to have students add their own comments and learning tips on pronunciation, translations into any of the African languages, etc. An alphabetical index provided easy access to the required word. Wherever possible, a link to a relevant online MoM-SA page was added (see Figure 5). All the development stages were discussed with the South African lecturer and the lemmata were translated by a native speaker of Spanish who is familiar with the project.
Figure 5. An Example of a Page from the Pocket Picture Dictionary
In August 2013, this concept was introduced to a class of eight medical students who had just completed their medical training in Cuba. The dictionary was offered to them as an interactive booklet and students were invited to take part in the process of developing content for the dictionary. Since only five medical topics, i.e., body parts, garments, equipment, diseases and organisation, were included, every student received one paper version of the dictionary and was invited to use the space provided to add terminology, images and suggestions on a weekly basis. In this way they could become co-owners of the dictionary of an on-going project, as described in the introduction of the booklet, shown in Table 1.
Table 1. Introduction to MoM Booklet
Additionally, during three lessons, five minutes were spent on providing feedback on the existing booklet as well as on brainstorming ideas concerning the extension of the list. All of the students’ contributions were collected at the end of the course and integrated for the second version of the dictionary. In line with what is indicated above, as a thank-you they received an updated and extended version of the list that acknowledges them as contributors to the dictionary.
Students’ Findings and Experiences
Judging from the students’ willingness to participate in learning activities in class at the start of the 20-hour course on the one hand, and from their spontaneously-asked questions related to vocabulary and grammar on the other, the lecturer concluded that her students are motivated to learn how to communicate in Afrikaans within a professional medical context. During class conversations, the students showed their motivation by spontaneously consulting the dictionary, as well as by adding information to it.
Nevertheless, as expected, due to the limited number of words recorded in the dictionary (135 only), the shortcoming of the materials developed so far was evident, once the students left the safety of their classroom. After the first 10 hours of attending class, students spent a week observing surgery in the Gynaecology Department of the hospital and were involved in conversations with the patients on topics ranging from administering medication to discussing a cancerous tumour. Afterwards, students revealed that they were often at a loss trying to communicate with patients in Afrikaans. Confirming the potential usefulness of the pocket-size dictionary, while observing or being on duty in the hospital, the students added more words and suggestions to the dictionary-in-progress. The notes that the students made in the dictionary were both in English and Spanish, possibly an indication that the students were still in the process of moving from and between Spanish, the Cuban language of instruction, to English, their chosen South African language of instruction. Most students added vocabulary such as the names of diseases, or symptoms such as “itching” or explained that they would like vocabulary related to systems review, e.g. the muscular system and the digestive system. One student also requested basic sentence structures, such as questions and instructions: “Short of breath. How do you ask ‘short of breath’?” This comment underlines that students experience a need for language support when they have to communicate with patients. Although this kind of communication support is not part of the dictionary, students can contribute to and enrich the teaching based on their own experience. Scenarios following the consultation timeline are part of the online MoM-SA, but given the limitations of classroom contact time, not all can be dealt with in class. We can only hope that through the teaching we have established a framework for ongoing and continuous learning.
When asked to comment on the dictionary, one student replied: “It helps you to find a word when you are in a hurry”. At the end of the course the dictionaries were collected in and the students’ notes analysed. Most students extended the word list by adding names of diseases and more symptoms to the lemmata. There seems to be a correspondence between the number of notes added to the dictionary and the learning gain of the student. A higher number of notes in the dictionaries seems to correlate positively with a consistent increase in proficiency throughout the course. It seems therefore that the dictionary-in-progress contributes to learning. Moreover, the focus on the tool seems to reinforce students’ motivation as shown in the course evaluation. As part of the evaluation process, students indicated their degree of (dis)agreement on a four-point Likert scale. In the present context, it is relevant to note that an overwhelming majority of 86% (strongly) agreed that their “Afrikaans vocabulary has improved” and that the materials are viewed as being relevant to their needs. However, almost half of the students felt that more time should be allocated in their training programme towards the Afrikaans communication course and they expressed the hope that their medical vocabulary knowledge would improve.
The Cuban-trained South African medical students clearly have different needs from the other SA medical students attending courses in Afrikaans which we tried to cater for. To the current group of students, who are co-authors of the pocket dictionary, process has indeed become content (Legenhausen, 2013). While the learners were using and compiling the word list, they had to investigate their needs both as students in a South African learning environment and as future medical professionals. The students’ learning needs clearly came to the fore and were emphasized when they were in real-life professional situations that depended on effective communication. In one way, of course, these pre-professionals already have acquired an identity as medics; however, they have to express their professional identity in line with the new environment. To this end, they need a tool that gives them access to the language they need; therefore, when they were contributing to the word list, they were at the same time also contributing to the formation of their own SA-identity (as medical professionals) as they experienced it on ward rotation. In turn, these needs had to be translated to the content and structuring principles of the dictionary, which had to be adapted and developed as the course content continued, because these experiences continuously informed the students’ needs. The on-going process of contributing to the dictionary had the added benefit that, in a very simple but effective and visible way, it suggested to students that the (communication course) content was growing as their learning needs developed and that learning is therefore a continuous and dynamic process.
Hopefully, these students will benefit to some extent, during the rest of their training and possibly into their professional careers, from the use of the pocket dictionary.
The Future of the Wordlist Booklet
Based on the end-of-course feedback from the students, the dictionary will be extended and developed further to include more topics and words. Contexts that will be included are related to systems’ review (symptoms and illnesses), which are components of MoM-advanced and already exist for the European languages, but will have to be developed for Afrikaans.
Moreover, we intend to include QR codes. These are machine-readable codes consisting of an array of black and white squares, typically used for storing URLs or other information for reading by the camera on a smartphone. Since most students have access to a smartphone and most only have access to a computer while on campus, we expect this to be a useful add-on next to the urls in the dictionary in order to refer the students to relevant online/mobile scenarios within the MoM-SA course. The revised paper edition of the dictionary will be tested in 2014 and students’ attention will be drawn to the possibilities of the online vocabulary components and contexts.
At the same time, the MoM team is studying the potential to include the dictionary in the already existing online MoM-SA materials, extending them with more words and graphics online. The online dictionary could include audio examples and function as a new medium and additional learning platform within MoM-SA online.
Finally, since MoM-SA does exist as an online, but also as a mobile tool, it is worth considering turning the dictionary component into an app. This opens some perspectives because smartphone apps would always be at hand, or, as one of the Cuban-trained students explains in her feedback on the future of the dictionary: “I would use the dictionary because sometimes I forget a word in english but I remember it in spanish. It would be more convient for me to have it as an app coz it mininmizes the chances of me losing the dictionary and its more accesible that way (sic.).”
Concluding Remarks
Language support systems, such as the pocket picture dictionary, may also have a beneficial role to play in supporting the Cuban-trained students’ re-entry process (see Van de Poel & Gasiorek, in press, for a detailed analysis). Ideally, tools of this kind should help students save mental energy (i.e. by removing the burden of constructing language learning materials on their own and relying on the community for shared input), which should also allow them more available mental resources to cope with the challenges of re-entry to South Africa and to engage more fully in other areas of their pre-professional life. Additionally, to the extent that these materials help students address the linguistic and communicative challenges they face, they may also help these students build confidence in their academic and (pre-)professional lives. Finally, if these communication support tools are developed as online/mobile resources, they will have the potential to foster the learners’ autonomous and continuous learning and training in a clinical context, which could provide benefits well beyond the students’ initial return and orientation programme.
Notes on the contributors
Kris Van de Poel, University of Antwerp, Belgium & North West University, South Africa, has taught and studied applied linguistic topics for the past thirty years. As MoM’s coordinator, MoM-SA is of special interest to her since it marries issues of language for occupational as well as academic purposes.
Christine Fourie is a freelance lecturer at Stellenbosch University’s Language Centre, South Africa, while doing a PhD on the role of the teacher in blended learning at the University of Antwerp, Belgium.
Karen Seberechts is a junior researcher at the University of Antwerp, Belgium and has just finished a Master’s thesis on autonomous vocabulary learning.
References
Gasiorek, J., & Van de Poel, K. (2012). Divergent perspectives on language-discordant mobile medical professionals’ communication with colleagues: An exploratory study. Journal of Applied Communication Research, 40(4), 368-383. doi:10.1080/00909882.2012.712708.
Graham, R. G. (2006). Blended learning systems – definition, current trends, and future directions. In C. J. Bonk & R. G. Graham (Eds.), The handbook of blended learning: Global perspectives, local designs (pp. 3-21). San Francisco, CA: Pfeiffer.
Health Care in South Africa. (2012, July). SouthAfrica.info. Retrieved from http://www.southafrica.info/about/health/health.htm#.UluRDbwWStc
Hewett, D. G., Watson, B. M., Gallois, C., Ward, M., & Leggett, B. A. (2009). Communication in medical records: Intergroup language and patient care. Journal of Language and Social Psychology, 28, 119-138. doi:10.1177.0261927X08330612
Hirsch, M. (2013). SA-Cuba medical programme criticized. Retrieved from http://www.iol.co.za/news/south-africa/sa-cuba-medical-programme-criticised-1.1545474#.Uod3hyjR6MM
Legenhausen, L. (2013, September). Learner autonomy as a response to the challenges of educational inclusion. Paper presented at the IATEFL Learner Autonomy Special Interest Group local conference, Hannover, Germany.
Little, D. (1991). Learner autonomy, 1: Definitions, issues and problems. Dublin, Ireland: Authentik.
Medics on the Move. http://www.medicsmove.eu
Silverman, J. D., Kurtz, S. M., & Draper, J. (2006). Skills for communicating with patients. Oxford, UK: Radcliffe.
Szkudlarek, B. (2010). Re-entry—A review of the literature. International Journal of Intercultural Relations, 34(1), 1-21. doi:10.1016/j.ijintrel.2009.06.006
Stewart, M. A. (1995). Effective physician-patient communication and health outcomes: A review. Canadian Medical Association Journal, 152(9), 1423-1433.
Swanepoel, P., & Van de Poel, K. (2003). Theoretical and methodological pluralism in designing effective lexical support for CALL. Computer Assisted Language Learning, 16(2-3), 173-211. doi:10.1076/call.16.2.173.15878
Van de Poel, K., & Gasiorek, J. (in press). “We feel stupid and we shouldn’t”: Towards developing a support system for Cuban-trained medical students. Per Linguam.
Van de Poel, K., & Seberechts, K. (2013). A pocket picture dictionary. English (EN)/ Afrikaans (AFR) / Español for Cuban-trained medical students. Bloemfontein, South Africa: ICELDA.
Watson, B. M., Hewett, D. G., & Gallois, C. (2012). Intergroup communication and health care. In H. Giles (Ed.), Handbook of intergroup communication (pp. 293-305). New York, NY: Routledge.
Notes
[1] The South African MoM-team is lead by Kris Van de Poel and Tobie van Dyk. The project is undertaken with financial support from ICELDA and the research unit for Applied Language Studies at the University of Antwerp in Belgium.
[2] At Stellenbosch, about ten Cuban-trained students take part in the annual intensive programme.